CentraMed’s Payment Discrepancy & Recovery Software
CentraMed’s solution portfolio now includes a “stand alone” software module specifically designed for managed care payment discrepancy recovery – including both defensive and offensive audit strategies.
CentraMed’s team has been providing audit fulfillment services and solutions for decades, and our subject matter expertise is substantive. In moving our solutions to the web, and adding a layer of business intelligence, we are now able to pre-query and screen managed care claims – this means an efficiency gain of 10X and an improved use of time on collection, follow up and process improvement activities.
Your managed care analysis and management team will have the ability to:
- Automatically import pre-queried claims meeting your requested criterion, e.g., open or closed balance claims;
- Use automatic reimbursement prompts for validating payment discrepancies
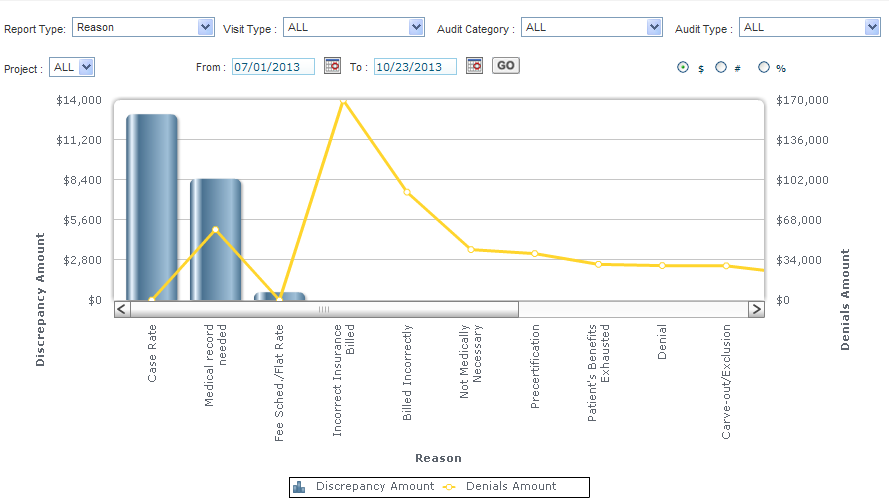
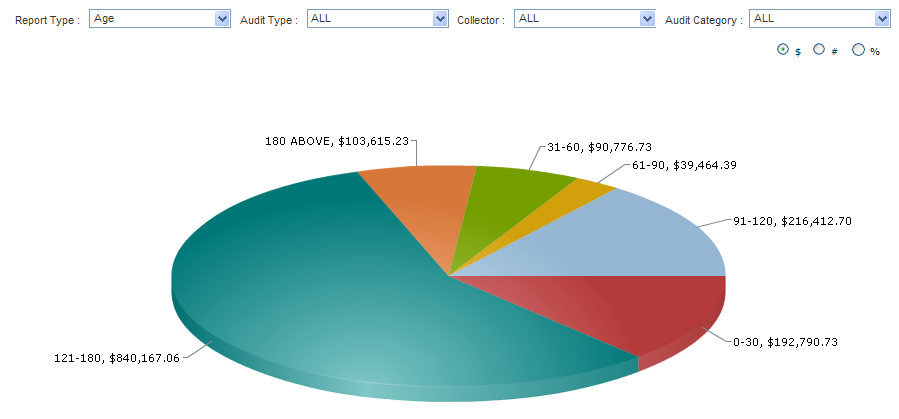
- Easily document to comprehensive metrics and analyses prompts, e.g., discrepancy type, service type, payor, plan, and more;
- Implement and monitor productivity standards for both auditors and collection team members;
- Prioritize work queues based on volume; and
- Run focused and summary reports from our robust library with customization capacity.
This is a subscription solution; once implemented, all your analysts need to do is log on and go! We provide ongoing data, training, and help support for as long as you need.
Fast, efficient, reasonably priced, sustainable and profitable!
For more information, including an ROI analysis or demo, please contact CentraMed at (760) 476-0077 or info@audacthealth.com.



Speak Your Mind